Massachusetts is facing an explosion in its 85-and-over population by 2050 at a time when nursing homes are closing and the ones still operating are struggling to secure higher public payment rates, access capital funding, and attract and retain workers, according to a new task force report.
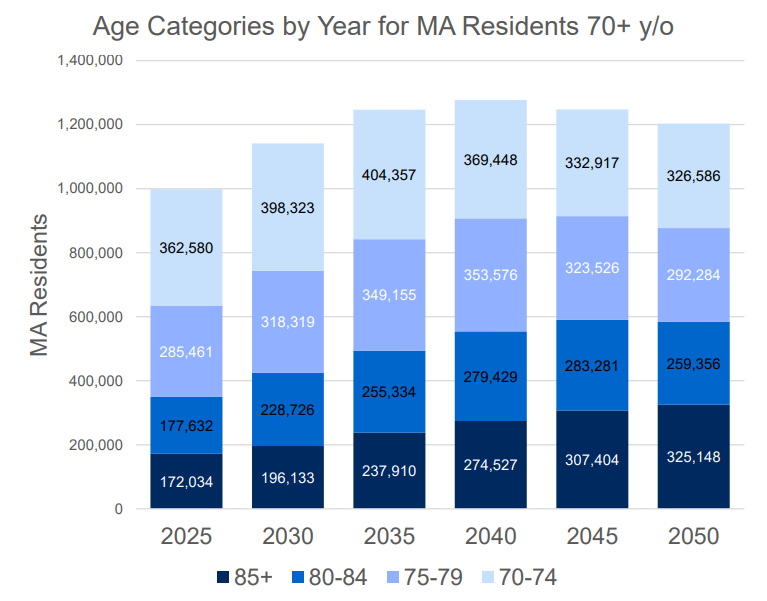
Massachusetts is currently home to 172,034 residents who are 85 and older, a figure that is projected to swell to 274,527 in 2040 and 325,148 by 2050, according to estimates from the UMass Donahue Institute.
Thirty-four nursing facilities have shuttered across Massachusetts since 2020, translating into the loss of 3,515 beds, according to the report from the Viability and Sustainability of Long-term Care Facilities Task Force. The panel was created through the 2024 long-term care reform law.
The closures have occurred in Great Barrington, Montague, Norton, Weston, Williamstown, Agawam, Brookline, Lowell, Newton, Revere, Wareham, Worcester, Attleboro, Boston, Dedham, Gloucester, Needham, Quincy, Rowley, Chicopee, Springfield, Westfield, Dennis, Stoneham, Concord, New Bedford, Stoughton, Bridgewater, Northampton and Lynn.
The report lists the 2021 closure of the 164-bed Beaumont Rehabilitation and Skilled Nursing Center in Worcester as among those which have shuttered since 2020.
The state’s existing portfolio of long-term facilities includes 348 nursing facilities, with 39,899 beds; 273 assisted living facilities, with 19,093 beds; and 58 rest homes, with 2,002 beds. Massachusetts previously had 74 rest homes, for a total of 2,404 beds, in 2015.
In 2023, nursing facilities posted a total margin median of negative 1.6%, compared to negative 3% in 2022, the report said, citing Center for Health Information and Analysis data. In both years, more than 58% of facilities reported losses. Facilities in central Massachusetts had the highest median total margin of 0.7%, while those in metro Boston had the lowest median total margin of negative 4.8%.
In a key research objective, task force members investigated demand for long-term care beds over the next five and 10 years and found that the Executive Office of Health and Human Services “estimates that there will be sufficient capacity until 2034.”
The task force had “extensive discussion about drivers that would cause a bed shortage to occur earlier or later than 2034.” Variables include facility closures, bed access challenges in certain regions, state investments in home- and community-based care, and new care delivery models like offering skilled nursing in home settings.
Massachusetts could experience a deficit of skilled nursing beds by 2035, projections show. The report notes that the volume of residents requiring dementia care will also rise during the next decade, with the prevalence of Alzheimer’s expected to increase by 25%.
As policymakers look to shore up long-term care infrastructure to keep up with demand from a rapidly growing older population and counteract the spate of recent home closures, the task force offered recommendations to ensure adequate rates, bolster access to capital funding, and invest in the direct care workforce. The panel examined the demand for care, staffing challenges that could be exacerbated by a loss of immigrant workers due to shifting federal policies, and strategies to improve the quality of care, among other issues.
Rates are a perennial issue on Beacon Hill, as health care industry leaders vie for more state funding with the hope of improving the quality of care and making strides in workforce recruitment and retention.
“Ensuring funds are appropriated to support adequate rates is the most important issue for the legislature to focus on to ensure quality care and avoid further skilled nursing facility and rest home closures,” the report states. “A long-term care facility’s ability to invest in quality resident care and staff is directly tied to adequate funding.”
The Legislature could direct EOHHS and CHIA, alongside independent researchers, to probe the rate setting process, the task force recommends.
In rest homes, payments for residents who are on public assistance lag “actual care costs” by more than $20 daily, said Ron Pawelski, president of the Massachusetts Association of Residential Care Homes. In skilled nursing facilities, that gap is closer to $40, Pawelski said in a memo attached to the report.
Long-term care facilities have pegged staffing as “one of their biggest challenges,” and many nursing homes lack enough workers to keep up with their licensed bed capacity, according to the report. While there are 38,782 licensed beds across all nursing facilities, only about 38,000 are staffed.
Nursing homes must hire more than 5,000 direct care workers amid rising demand, the report says. And to comply with staffing and hourly minimum requirements to provide adequate nursing care, facilities “would need to add on average 744 nurses working 8 hours, of which 244 must be RNs, each day across Massachusetts,” the report says.
The state should invest in Medicaid rates for nursing facilities and Department of Transitional Assistance rates for rest homes, with the aim of paying a “more competitive wage for frontline staff, 90% of whom are women and more than 50% of whom are people of color,” the task force recommends. Policymakers should also invest in career advancement opportunities, including for resident care assistants, certified nursing assistants, certified medication aides, licensed practical nurses and registered nurses.
A number of state workforce initiatives are already underway, including allowing the CNA exam to be taken in Haitian Creole, Spanish and Chinese; a 200-hour training program for CNAs and home health aides for non-native English speakers; and a career pathway program that covers tuition and expenses for direct care staff looking to become LPNs.
The task force says Massachusetts must also address the aging infrastructure at long-term care facilities. But for now, nursing facilities and rest homes struggle to access capital “for critical maintenance and large capital investments, to address things such as roof replacement, window replacement, heating and air conditioning,” the report says.
“Facilities need access to capital to plan for capital needs and to avoid emergency repairs, current rates do not allow for adequate capital reserves,” the report says. “Incentives in the rate-setting method and staffing regulations encourage facilities to prioritize staffing and defer maintenance, given available resources. Numerous nursing facilities and rest homes have closed over the past several years due to deferred maintenance issues.”
Massachusetts could roll out grant programs, or offer zero- or low-interest loans, to connect facilities with capital funding, the task force suggests.
Among other strategies to improve care at long-term care facilities, the task force recommends slashing avoidable hospital admissions, reducing the use of antipsychotic medication, implementing strategies to reduce falls, and pursuing “person-centered care strategies” to help with individual resident outcomes.