Tens of thousands of Bay Staters could lose subsidized health insurance through the Massachusetts Health Connector and premiums could rise for most other members under a suite of reforms in the U.S. House-approved reconciliation bill that Gov. Maura Healey dubbed “devastating.”
For months, officials and health care activists have been warning about major impacts to MassHealth from the Medicaid changes sought by Republicans in Congress, who want to fund tax cuts and rein in what they describe as wasteful spending.
But the sweeping package that cleared the U.S. House last week features many other provisions that could also impact state-run health insurance marketplaces, including limitations on tax credit eligibility for some immigrants and a shorter open enrollment period.
Massachusetts Health Connector Executive Director Audrey Morse Gasteier said as many as 100,000 people — roughly a quarter of all who get their health insurance through the marketplace — could lose their coverage.
Taken alongside the roughly 150,000 other people who would lose MassHealth eligibility, Morse Gasteier said the House-approved bill would effectively double the number of Bay Staters without health insurance.
“[That] is just such a heartbreaking and catastrophic future to contemplate after Massachusetts, for nearly 20 years, has been at the forefront and really all in on making sure everybody in Massachusetts has health coverage,” Morse Gasteier told the News Service.
A Connector spokesperson said the most recent U.S. Census data estimates about 2.6% of Massachusetts residents are uninsured. State law requires Massachusetts residents to be insured, or pay a tax penalty.
A June 2024 Center for Health Information and Analysis report estimated 1.7% of Massachusetts residents reported being uninsured in 2023, which translates into about 116,594 residents. Nearly 90% of the uninsured were adults aged 19 to 64, four-fifths were male, and two-thirds of the uninsured had a family income below 300% of the federal poverty level.
Under the House bill, premiums are also likely to rise for those who remain insured through Connector plans, Morse Gasteier said. She also forecast a major financial impact, saying the policy changes in the bill and the expected end-of-year expiration of tax credits to help reduce premiums would cost residents and the state a combined $750 million per year.
The sweeping federal legislation, which also touches on immigration, artificial intelligence and food aid, features numerous eligibility and spending reforms affecting Medicaid programs and health care marketplaces under the Affordable Care Act.
Hannah Frigand, senior director of HelpLine and public policies at Health Care for All, described the package as a “backdoor repeal of ACA marketplace coverage.”
“It seems like almost the intent of some of these decisions in here is to make it more difficult for the state to provide meaningful access to affordable coverage to individuals,” she said. “It’s so directly attacking [ACA marketplace coverage] in multiple ways to make it less affordable and less accessible.”
Kaitlyn Kenney Walsh, vice president of policy and research at the Blue Cross Blue Shield of Massachusetts Foundation, said the policies “will have significant deleterious impact on people getting health insurance coverage through the Health Connector who have come to rely on that coverage.”
U.S. House Speaker Mike Johnson has targeted July 4 as the deadline to get a final bill to President Donald Trump’s desk in order to provide tax relief “as soon as possible.”
“We have a very delicate equilibrium that we reached on here,” Johnson said last week. “A lot of work went into this to find exactly the right balance.”
It’s not clear how the U.S. Senate will respond to the proposal, and a handful of Republicans have voiced concerns that the measure either does not do enough to reduce the national deficit or would harm Medicaid recipients.
One of the most significant changes in the bill limits the eligibility of many immigrants for tax credits to help reduce the cost of health insurance plans through state-run marketplaces like the Connector.
Under the bill, only lawful permanent residents, Compact of Free Association (COFA) migrants or certain immigrants from Cuba would qualify for subsidized marketplace coverage. Morse Gasteier said that change would cut 55,000 to 60,000 other legally present immigrants in Massachusetts, like those seeking asylum, refugees and those waiting for Medicaid eligibility to begin, from the Health Connector’s ranks.
The federal bill would create new verification requirements for marketplaces, preventing enrollees from receiving tax credits toward premiums or cost-sharing reductions until their eligibility is confirmed, according to a detailed analysis by health policy nonprofit KFF.
It would also largely limit auto-renewals and mandate marketplaces hold annual open enrollment periods from Nov. 1 to Dec. 15, about five weeks shorter than the Health Connector has offered for more than a decade.
“The bill would make it so that people need to verify information before they even see that they qualified for a lower-cost option, which will effectively mean that many people will just think they don’t qualify and will not even try to submit documents because they think, ‘I’m not eligible for subsidized coverage,’ which will prevent many people from actually enrolling into insurance,” Frigand said.
Morse Gasteier said the additional hurdles will “make the process of obtaining and keeping coverage harder for everybody.” If fewer people are covered, she said, the remaining insured population will become higher-risk and higher-cost as a result.
“With respect to the administrative burdens and the red tape and the needless kind of sludge that this bill would erect for people that are trying to get and keep coverage, we would expect — just based on the way health insurance works and the way human behavior operates — younger and healthier people will probably not go through the trouble of making their way through all of these hoops,” she said.
And when Bay Staters get ill or injured while not carrying insurance, the eventual health care costs will be “borne by our entire health care system and passed on to premium payers through hospital debt that needs to be spread across the rest of the population,” Morse Gasteier said.
Some of the impact could come not from the reconciliation package itself, but from congressional inaction. The pandemic-era American Rescue Plan Act and Inflation Reduction Act expanded ACA tax credits that help subsidize premium costs, and those credits are set to expire at the end of the year.
The federal bill on the move does not extend those credits.
“It’s been a really significant help to the state, to the ConnectorCare program and to individuals who are just over that cliff for eligibility for those premium subsidies under the Affordable Care Act baseline,” Morse Gasteier said.
State law requires most adults who can afford it to have health insurance coverage for the entire year or pay a tax penalty. Many Bay Staters get health insurance through their employers, and MassHealth provides coverage to those with low incomes or disabilities.
The Connector offers plans for individuals who do not qualify for MassHealth and also cannot get covered through their employers, such as people working multiple part-time jobs or gig workers, as well as a subsidized ConnectorCare Program.
Healey described the Connector’s membership as “people who make just a little bit too much to qualify for MassHealth but are still just getting by.”
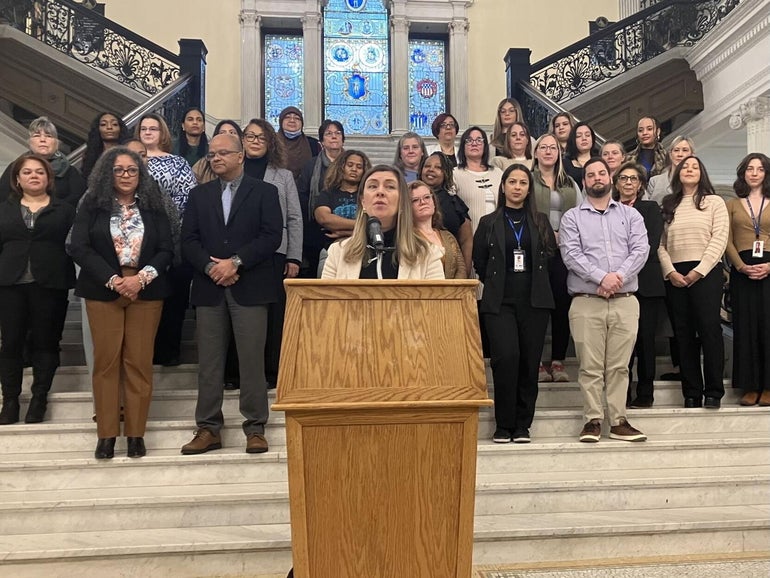
“Who are these people? There are a lot of people running small businesses. They’re people who are self-employed,” Healey said at a Tuesday event where she warned about major health care impacts from the reconciliation bill. “The Republicans and Donald Trump want to slash funding for the Health Connector as well, and this is going to drive up premiums, force 100,000 families to go without coverage. So you can see, the proposed cuts, if they go through, they’re devastating for Massachusetts residents, for families, for employers, for our economy, for people across the state.”
Lawmakers and Healey agreed on a pilot expanding income eligibility for the ConnectorCare program from 300% of the federal poverty level to 500%. Both Healey and the House in their fiscal 2026 budget bills proposed extending the pilot another year, but the Senate did not include the extension in its redraft.
Sen. Cindy Friedman, co-chair of Senate Committee on Steering and Policy, noted Wednesday that the pilot is available, albeit temporarily.
“I would like you to tell your patients that, while it lasts, the Connector in Massachusetts has raised their subsidies to 500% of the poverty level,” Friedman told the CEO of an organization that operates sexual and reproductive health clinics. “And that has made a real profound difference in people getting into health care.”