About 76,000 people have been removed from the MassHealth rolls since March, and officials continue to forecast the biggest impacts are around the corner as a massive reevaluation of eligibility ramps up this fall.
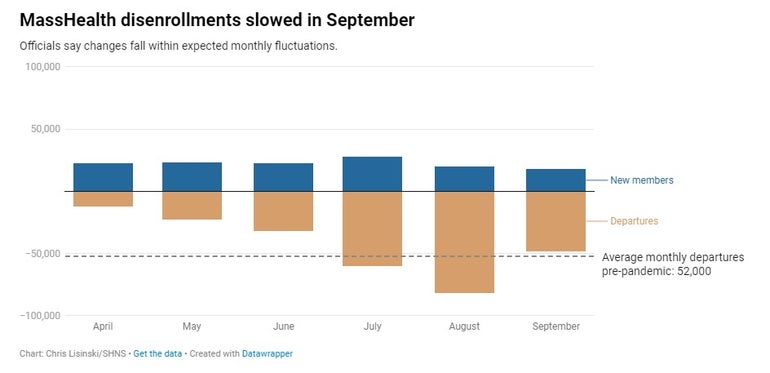
MassHealth published the latest monthly summary of its year-long redetermination effort Friday, showing that another 48,000 people lost MassHealth coverage in September. That was offset by about 18,000 new enrollees and 6,300 people who rejoined the publicly funded health insurance program after previously losing coverage.
September saw fewer disenrollments than in either of the previous two months — and less than the average monthly amount before the COVID-19 pandemic — but officials said they view the change as “normal fluctuation.”
“You will see an increase in disenrollments as we head into the fall and winter. That is typically the time of the year when we see the most disenrollments because we time many of our renewals with open enrollment with the [Massachusetts Health] Connector,” Assistant Secretary for MassHealth Mike Levine said. “We know that in the months ahead, beginning in October, we really are going to see a pretty steep uptick in disenrollments.”
For the first time, officials on Friday also offered a glimpse at how many Bay Staters retained MassHealth coverage after being subjected to redetermination. About 60 percent of MassHealth members younger than 65 who went through a full reassessment remained enrolled in the program, which combines Medicaid and the Children’s Health Insurance Program under a single umbrella.
“This does not mean that we expect 40 percent of members to lose coverage,” MassHealth Chief Operating Officer Elizabeth LaMontagne said, noting that the estimate excludes populations that are “highly likely” to renew and that more older adults in particular are expected to be automatically renewed in the coming months.
Massachusetts is now six months into a year-long campaign to reassess eligibility for all 2.4 million people who were on the MassHealth rolls at the outset. The Healey administration originally projected the effort would decrease enrollment by a net 300,000 to 400,000 members, saving $1.9 billion in fiscal year 2024 state funds that could be spent elsewhere. Officials said Friday those estimates have not changed.
The federal government prohibited kicking people off of Medicaid during the pandemic, but that policy ended this year, requiring all 50 states to embark on a similar redetermination of their programs.
In Massachusetts, disenrollments so far are about evenly split between people found no longer eligible and members who were kicked off because they failed to provide the state with enough information.
That diverges from the national outlook. Across all states, an average of 72 percent of Medicaid members have lost coverage for procedural reasons, according to data tracked by nonprofit health policy group KFF.
Levine said he is not yet concerned that about half of the Massachusetts residents booted from MassHealth lost coverage for failing to submit enough information because the figure likely captures many people who have not used the publicly funded insurance for months or years.
Someone who lost their job — and therefore their employer-sponsored health insurance — in April 2020 and joined MassHealth might have found a new job with insurance benefits just a few months later, he said. But the federal pause on disenrollments would have kept them in the MassHealth pipeline until the current redetermination.
“If I am on MassHealth, and MassHealth pings a data set and sees that my income is too high for Medicaid, I get a blue envelope. I am not going to bother filling out that blue envelope and sending it back in to tell MassHealth that I’m not eligible,” Levine said. “That gets counted as a procedural termination because we just don’t get data back from that person.”
For now, Levine said he does not view a 50-50 split between people removed because they are no longer eligible and people removed for paperwork reasons as a signal “that a bunch of people are going to be rolling off without insurance.”
MassHealth officials are closely tracking the number of people who rejoin MassHealth shortly after being removed.
“To me, that is the signal, right? If a lot of people are returning very quickly, that means that there are people who are eligible who are missing their notices and not taking action,” Levine said.