The troubles, though, date back to 2019, even before the COVID pandemic, when the Association of American Medical Colleges reported hospitals in the country were understaffed by as many as 20,000 doctors.
Get Instant Access to This Article
Subscribe to Worcester Business Journal and get immediate access to all of our subscriber-only content and much more.
- Critical Central Massachusetts business news updated daily.
- Immediate access to all subscriber-only content on our website.
- Bi-weekly print or digital editions of our award-winning publication.
- Special bonus issues like the WBJ Book of Lists.
- Exclusive ticket prize draws for our in-person events.
Click here to purchase a paywall bypass link for this article.
The emergency room at UMass Memorial Medical Center’s University Campus in Worcester strains under the pressure on a Friday evening in late October. People wait to check-in, a line forms along one wall as they wait to go through the metal detector for an initial assessment. One nurse can be heard talking about how he has a place to live, even a mortgage, but he barely knows what it looks like because he’s never home.
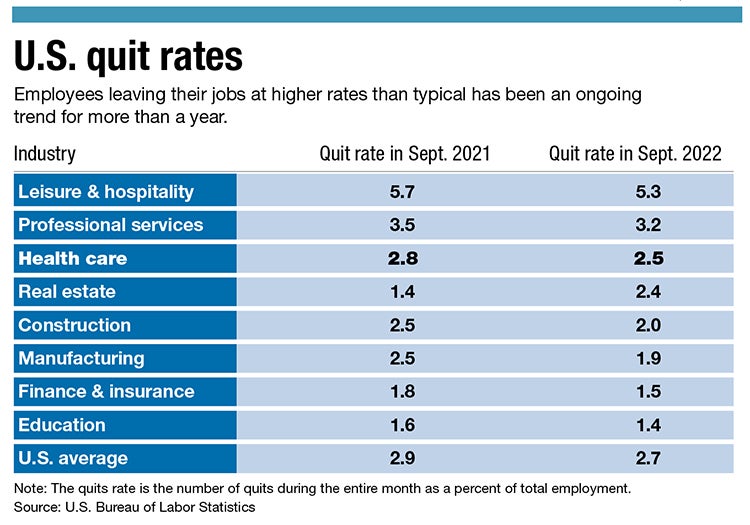
According to the U.S. Bureau Of Labor Statistics, 527,000 U.S. healthcare workers quit their jobs in August and preliminary numbers for September show another 521,000 workers quit. The trend is marginally down since September 2021 when 575,000 workers left their jobs. The troubles, though, date back to 2019, even before the COVID pandemic, when the Association of American Medical Colleges reported hospitals in the country were understaffed by as many as 20,000 doctors. Incredible Health, a San Francisco-based healthcare hiring agency, said 34% of nurses plan to leave their current position by the end of 2022.
“We went into the pandemic behind the 8 ball and didn’t have enough nurses or help,” said Colleen Wolfe, a nurse in the surgical acute care unit at UMass Memorial Medical Center’s Memorial Campus, who has been with the hospital since 1996. “When all hell broke loose in the pandemic, we lost our teams, and teams gave us hope.”
The number of U.S. workers reporting feeling burned out very often or always went above 30% in February for the first time since the start of the coronavirus pandemic, according to a survey from Washington, D.C. data firm Gallup. But numbers are higher among healthcare workers, who toil in a system where hospital workers from doctors to nurses to custodians and everyone in between have been put under enormous pressure and decided to call it quits.
Susceptible to burnout
In a lot of jobs, people can check out after work. They don’t need to keep up on all the latest news once their hours are completed. But, for people in health care, the world of keeping people healthy and safe as well as the technology used to do that, never stops evolving. To keep up to date on all of that requires physicians and nurses stay on top of medicine outside of work. And that can weigh on the people trying to keep everyone else safe.
In November 2021, Dr. Victor Dzau, president of the National Academy of Medicine and the former president and CEO of the Duke University Medical Center, told the audience of a U.S. News & World Report webinar even before the pandemic physicians were two times more susceptible to burnout and about 40% of physicians surveyed reported depression and suicidal ideation.
Since the pandemic, though, the numbers have risen. Dzau said 60% to 75% of clinicians reported symptoms of exhaustion, depression, sleep disorders, and PTSD. Pair that with 20% of healthcare workers quitting, and the issues exacerbate themselves.
All of this is what Dr. Shlomit Schaal is attempting to combat as the president of the UMass Memorial Medical Group, which is the nonprofit group of primary care and specialty providers for the larger healthcare provider parent organization UMass Memorial Health.

“The problem with us is that we are in healthcare and no one wants a physician to quiet quit on them,” Schaal said. “You don't want the physicians to do the minimum that they can because this is a profession of continuous learning, and medicine is always changing. I'm an eye surgeon, and nothing I do today is the way I was taught because medicine has been changing and progressing so fast.”
Schaal’s focus is on the 1,200-plus physicians in her group. She wants them to feel the value of being a doctor. She wants them to be reminded of why they took on this job in the first place and the moral compass that led them to want to help, because even in the darkest of times they’re helping. That’s their job. There are dark and long days. Zoom call days that feel like they never end.
Even as the strain increases as the population continues to grow and age – with the Baby Boomer generation now firmly at the age where it will need more care – the number of physicians in Schaal’s group has stayed the same since 2018. Schaal wants the physicians to remember that in the long run, the job is fulfilling. It’s about helping people and seeing people live and have a better life.
Schaal sees the hospital as one ecosystem. She wants everyone to know they’re part of this noble profession of keeping people healthy and alive.
“So it is reminding people we are here to improve other people's lives, to save lives,” Schaal said. “It is a continuous reminder that we need to put the purpose in front of everybody every day. And remind people that this is not just a job, not just a career. It is a purpose – a noble purpose, a noble profession.”

Nurses struggling
The ecosystem Schaal believes in, though, is struggling, as nurses are feeling the pull on the front lines.
Wolfe, the 26-year veteran of UMass Memorial Medical Center, can’t remember a time when nurses weren’t talking about needing more help. She has begun to see the impact the long hours and demanding work has taken on them.
“People looked at going above and beyond and recognized the toll it was taking on them,” Wolfe said. “I have to think about the impact on me and my family [of working more].”
For her, the weight of not taking off after work and forgetting her job can feel like it’s too much to handle, she said.
Miko Nakagawa spent 20 years as a nurse in the emergency department before moving over to the recovery room at the Leominster campus of UMass Memorial Health’s HealthAlliance-Clinton Hospital, and she feels the hospital has lost its place in the community, as it can no longer solely fulfill community needs. Instead, the hospital funnels patients to the bigger UMass Memorial hospitals in Worcester, she said, but with that delay time comes issues and sometimes patients can’t be seen because of a shortage of beds in Worcester. This puts nurses on the front lines of keeping people safe and healthy while not always being able to provide the necessary treatment.
“We don’t have the specialty doctors,” Nakagawa said. “We don’t have everything they have in Worcester.”
On top of that, Nakagawa feels the nurses there have been forgotten, which has led to quitting.
“We don’t feel listened to or valued,” Nakagawa said.
Finding hope
The issues aren't’ only for nurses, though. Dr. Peter Smulowitz, chief medical officer for the Milford Regional Medical Center, has seen it first hand and said the issues of morale are industry-wide.
“There have been issues caring for patients for the last three years – not enough staff or beds,” Smulowitz said.
This lack of resources gives doctors the feeling they don’t have any control over the situation, he said.
Doctors need systematic help to get out of the rut they're in, Smulowitz said. They’re behind and unable to keep up with patients and their needs. A 2021 Massachusetts health insurance survey from the Center for Health Information and Analysis reported 34% of Massachusetts residents reported difficulties accessing care in 2021, with 19% reporting difficulties getting an appointment with a doctor’s office or clinic as soon as needed.
Workers struggle after coming out of extreme moments in history, like a pandemic, said Kathy Kacher, president of Career/Life Alliance Services, Inc. in Minnesota and a workforce solutions specialist. In order to prevent worker fatigue, disengagement, burnout, quiet quitting, or whatever you want to call it, Kacher said more employers need to pay attention to what is happening.
“People come out from under the table to get back to the world,” Kacher said.
Now, though, instead of coming out of a pandemic and getting back into working extra long hours in the office, people learned what it was like to spend time with their families and close friends and don’t want to give that up again, she said. On top of that, people now know their value and are more aware of their mental health.
“The No. 1 issue [after the pandemic] was mental health,” Kacher said. “People are done. They’re tired.”
Kacher offered simple advice for companies to keep their employees engaged: Be kind and listen.
“Be generous, be empathetic, and have trust,” Kacher said. “If you can’t find the problem, you have to go to the front line and ask and listen.”
For its part, UMass Memorial has held town hall meetings for its employees so they can voice their opinions and be heard. On top of that, nurses and the hospital group agreed to new contracts that increase nurses’ benefits and wages, making the positions more desirable. This is all part of creating the ecosystem Schaal from UMass Memorial spoke about.
“We have idea boards where everyone can voice their opinions and give suggestions for improvement,” Schaal said. “I know my professional stuff – I know the books, I know the articles – but I don't know the everyday problems and what the solution is for them. Everyone at every level can solve something. We have what we call huddles, and [in] the huddles we have physicians, nurses, technicians, secretaries that participate in weekly huddles; and we can say, ‘You know what, we have this problem, and this is my suggestion on how to solve it.’”
For nurses like Wolfe, listening is key on more than one front. They’re asking patients to listen to them and not threaten them with physical or verbal abuse, and they’re asking the hospital to staff up with full-time nurses on teams they can grow and work with.
“We need hope,” Wolfe said, “that it’s going to change.”

