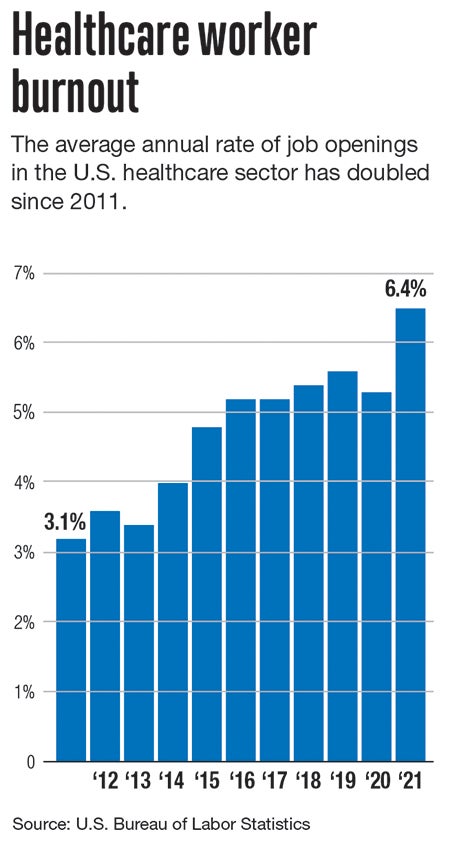
Burnout is nothing new in the healthcare field, but a mental health crisis among healthcare workers may be leading to startling staffing shortages as a third wave of the coronavirus pandemic threatens to overburden hospitals again.
Get Instant Access to This Article
Subscribe to Worcester Business Journal and get immediate access to all of our subscriber-only content and much more.
- Critical Central Massachusetts business news updated daily.
- Immediate access to all subscriber-only content on our website.
- Bi-weekly print or digital editions of our award-winning publication.
- Special bonus issues like the WBJ Book of Lists.
- Exclusive ticket prize draws for our in-person events.
Click here to purchase a paywall bypass link for this article.
Burnout is nothing new in the healthcare field, but a mental health crisis among healthcare workers may be leading to startling staffing shortages as a third wave of the coronavirus pandemic threatens to overburden hospitals again.
A quarter of U.S. healthcare workers have considered leaving their job since the pandemic hit, and 14% said they might leave the healthcare profession altogether, according to a January study from Washington, D.C. researcher Morning Consult.
“When the COVID pandemic struck, we were out buying ventilators and hiring traveling nurses. Now that we’re in the mental health pandemic that’s following, we don’t have the additional increase in resources to be able to keep up,” said Dr. Amy Harrington, who helps connect healthcare workers with UMass Memorial Health’s employee assistance program in Worcester for faculty health and well-being.

This stark reality in the healthcare industry is forcing providers to develop new programs to help caregivers, although they only go so far.
Nearly half the healthcare workers surveyed by Morning Consult reported the pandemic had negatively affected their mental health.
Harrington, who specializes in acute mental health and substance abuse issues, said she used to only receive a call once every couple of months. Now, she’s inundated with several calls a week.
COVID spiking again
Along with the grief of treating COVID-19 patients, healthcare workers are suffering from stressors at home, such as child care and increased isolation, and helping children with remote learning, said Harrington.
Fatigue is one of the most concerning aspects of the crisis, said Harrington, now with case numbers resurging and the community support seen in the early days of the pandemic dwindling.
“If anything, people are really starting to struggle now as we’re looking at the potential for another bad winter,” she said.
Meanwhile, demand for nurses – who make up the largest portion of the healthcare workforce – is expected to grow 7% in the next decade, a number likely to become higher if the pandemic worsens.
That means about 175,000 registered nurse positions will open, reflecting a significantly faster than average rate of growth, according to the U.S. Bureau of Labor Statistics.
Saint Vincent nurses strike
Staffing shortages, burnout, and a general worker exodus from the healthcare industry were already challenges before the pandemic, said Dominique Muldoon, a registered nurse who helped lead the Saint Vincent Hospital nurses strike starting in March.
“The issue started before the pandemic and was exacerbated,” said Muldoon. “During the pandemic, many nurses retired, other nurses who were not leaving the bedside left for hospitals with better pay, staffing, and working conditions. As a result, our staffing problems became that much worse.”
Staffing ratios is one of the predominant concerns voiced by striking Massachusetts Nurses Association union members.
Saint Vincent employees were offered free-of-charge access to counseling throughout the pandemic, according to the hospital’s communications department.
In April 2020, frustrations among staff grew when the hospital furloughed several nurses, tightening an already short-handed team.
A lack of communication between administrators and staff saddled nurses with even greater responsibility, both in creating a plan for the influx of patients and supporting each other emotionally, said Muldoon.
“Nurses really developed their own support system during COVID because we didn’t feel there was any kind of crisis management or recognition,” she said. “It was very frustrating that it felt like it was on us.”

Hospital solutions
Now, hospitals are getting creative about offering mental health services to their employees.
Dr. Steven Bird, a clinician experience officer at UMass, said there was very little programming when the clinician experience office opened in October 2019. Since then, Bird has helped launch a peer support network of caretakers and a wellness coaching service.
The office is jointly funded by UMass Memorial Medical Center, UMass Memorial Medical Group, and the UMass Medical School, all headquartered in Worcester.
As part of another initiative, a wellness coach travels by cart to nursing stations to offer in-unit support during tense moments at work.
“One thing we’ve learned is that the needs of people are largely work-unit dependent,” said Bird.
The clinician experience office is now focused on individualizing mental health care for specific units by developing programs meeting needs of workers in different settings, he said.
In Massachusetts, there are 121 designated health professional shortage areas, 10% of which are located in Central Massachusetts, according to the National Health Service Corps.
The Massachusetts Department of Mental Health helps manage MassSupport, which launched in the spring of 2020, to offer crisis counseling and community outreach, funded by the Federal Emergency Management Agency.
MassSupport is directed toward all Massachusetts residents, but includes healthcare workers as one of its primary groups for engagement, offering a crisis text line and a directory of contacts for mental health services.

