More than 12,000 people left MassHealth coverage in April, and top state officials expect those numbers to grow significantly in the coming months as the process of redetermining eligibility for about 2.4 million Bay Staters ramps up.
The Healey administration on Thursday outlined a new digital dashboard summarizing data from the first month of the redetermination process, which will decide how many people can remain on publicly-funded health insurance for the first time since the COVID-19 pandemic began.
About a third more people fell off the MassHealth rolls in April than in March, but despite the early impacts, overall enrollment saw a net increase because about 18,700 people joined the insurance program over the course of the month — a tally officials described as relatively routine.
Assistant Secretary for MassHealth Mike Levine described the topline MassHealth growth in April as “a little bit counterintuitive.”
Impacts from the gargantuan effort to figure out who is still eligible might not become clear for several more weeks because of the lag time involved in the first batch of redeterminations, Levine said.
“There’s not a lot to see in April because we were just getting started and we took a very measured approach in April to begin to select members for renewal,” Levine told reporters. “But if you got selected for renewal as a MassHealth member in April, if you do not respond or you respond but it takes us a while to process, you’re not going to see a coverage impact until more like the late May, early June timeframe.”
If a MassHealth recipient got selected for redetermination review on April 15, Levine said, the “blue envelope” mailed to them signifying that status might not arrive until April 20. Most members then get 45 days to respond to the state, plus another 90 days if MassHealth decides it needs more information, pushing back the decision date for future coverage status by several weeks.
Roughly 7,000 Bay Staters who lost MassHealth coverage enrolled in Massachusetts Health Connector plans, many of which are subsidized, since the redetermination process started, according to data published by the Connector.
“We’re really trying to come at individuals who are losing MassHealth eligibility from every possible channel at the individual level and big-picture as well,” said Health Connector Executive Director Audrey Gastier. “So we’re heartened to see that is bearing fruit so far.”
Those who lose MassHealth can also choose to participate in employer-sponsored coverage, if available to them. Officials said Thursday they might not be able to quickly detect commercial insurance enrollment trends related to redetermination.
Massachusetts law requires all residents to have health insurance or face tax penalties, though a small percentage each year go uncovered.
Officials have been expecting for months that the process of redetermining eligibility for MassHealth, which combines the state’s Medicaid and Children’s Health Insurance Program, will be enormously disruptive.
Early estimates pegged the number of Massachusetts residents who will lose MassHealth coverage at between 300,000 and 400,000, and Levine said Thursday it’s “too early to say” if the early data will alter those projections.
Federal continuous coverage requirements that had been in place since March 2020 expired, and states across the country are required to determine how many people on their Medicaid rolls — which grew significantly during the public health crisis — are still eligible. Medicaid rolls expanded during the COVID pandemic after scores of forced business closures. After an unprecedented wave of layoffs, employment levels have rebounded strongly.
In other states that kicked off the redetermination process earlier, the impacts have been significant so far. The Kaiser Family Foundation estimated Wednesday that more than 500,000 people have been booted so far in 11 states, nearly half of which are in Florida alone.
Levine said the experience elsewhere has “made us redouble our efforts” to connect with Bay Staters likely to be affected.
“Many states, particularly red states, took the opportunity to start early, and they’re seeing high levels of coverage loss two months ahead of us. I feel really good about the outreach efforts we’re doing,” he said, pointing to a door-knocking campaign that has reached 200,000 doors so far. “We are doing unprecedented levels of outreach, all of our community based organizations are engaged. Our ground game is really, really strong, and I think when you just look around the country, you’re seeing significant levels of people coming off coverage.”
The total MassHealth enrollment in April of 2.41 million is nearly 660,000 people larger than enrollment in February 2020, before COVID-19 hit. State budget-writers are counting on the process of redetermination to free up about $1.9 billion to spend elsewhere in fiscal year 2024, which begins July 1.
Over the course of April, the state opened redetermination cases for about 108,000 of MassHealth’s 2.4 million enrollees. MassHealth plans to launch about 150,000 more redeterminations per month to tackle the full field within a year, as required by federal law.
Levine said the administration hopes to publish data covering the month of May by June 20.
About 4,400 of the Bay Staters who departed the MassHealth rolls in April, or a bit more than a third of the total losses, reside in one of 15 “priority communities” where MassHealth sees the most members at risk of becoming ineligible. Those communities are Boston, Brockton, Chelsea, Everett, Fall River, Framingham, Lawrence, Lowell, Lynn, Malden, New Bedford, Quincy, Revere, Springfield and Worcester.
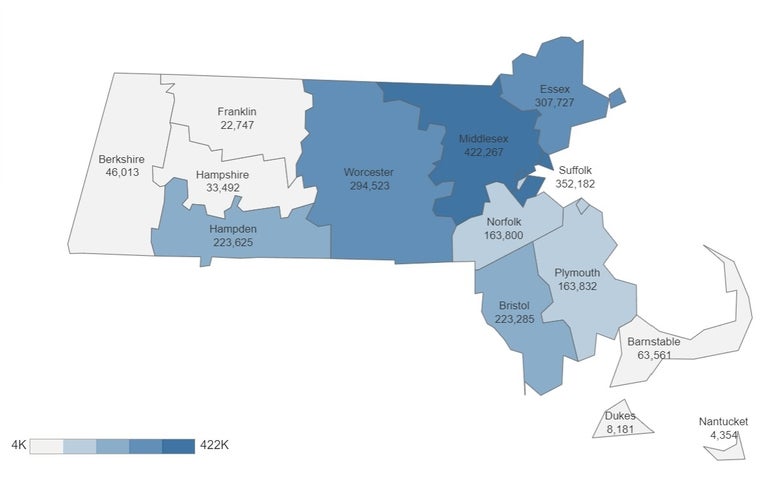
Middlesex County had the highest number of residents lose MassHealth coverage in April with 2,099, followed by Essex County with 1,414, Suffolk County with 1,389, Worcester County with 1,372, Bristol County with 925 and Hampden County with 853.
The decline was most concentrated among adults between the ages of 21 and 64, who made up nearly 60 percent of the more than 12,000 disenrollments. Bay Staters ages 20 and younger represented about 23 percent of April’s MassHealth losses, and adults 65 and older were 18 percent.
Levine said state officials are taking steps to support older residents, especially those who live in long-term care facilities, during the redetermination process. The “most important thing” older Bay Staters can do, he said, is ensure they have an authorized representative such as a family member or the facility where they reside.
“Every time then when we send a notice or renewal form to that individual, we send a carbon copy to the authorized representative or designee,” Levine said. “We send Mike Levine a renewal form, but Mike Levine lives at Smith Nursing Home — Smith Nursing Home gets all of that information and has staff who can help Mike Levine fill that out. That is above and beyond. And the good news is [for] a lot of our older adults and individuals with disabilities and other groups for whom this is an especially daunting process, having that authorized representative is just so key.”
Levine said older adults can also call the MassHealth customer service line, (800) 841-2900, and fill out their applications over the phone “with a trained and experienced customer service representative.”
Last week, the Healey administration announced MassHealth would direct $1.25 million in grant funding to 23 organizations to help train more counselors that will assist with renewals.