Drones dropping defibrillators from the sky, wearable watches that improve CPR, and telehealth services bringing medical expertise to any location in the world are just a few innovations seeking to improve medical outcomes in hard-to-reach areas.
Get Instant Access to This Article
Subscribe to Worcester Business Journal and get immediate access to all of our subscriber-only content and much more.
- Critical Central Massachusetts business news updated daily.
- Immediate access to all subscriber-only content on our website.
- Bi-weekly print or digital editions of our award-winning publication.
- Special bonus issues like the WBJ Book of Lists.
- Exclusive ticket prize draws for our in-person events.
Click here to purchase a paywall bypass link for this article.
Drones dropping defibrillators from the sky, wearable watches that improve CPR, and telehealth services bringing medical expertise to any location in the world are just a few innovations seeking to improve medical outcomes in hard-to-reach areas.
The COVID-19 pandemic had many negatives that irrevocably changed society; however, the crisis highlighted gaps in the healthcare industry now being addressed. One of these notable gaps was the lack of accessibility to healthcare services in rural areas. Lack of transportation combined with long proximity away from medical centers are some of the major hurdles residents in small towns must overcome to receive medical treatment.
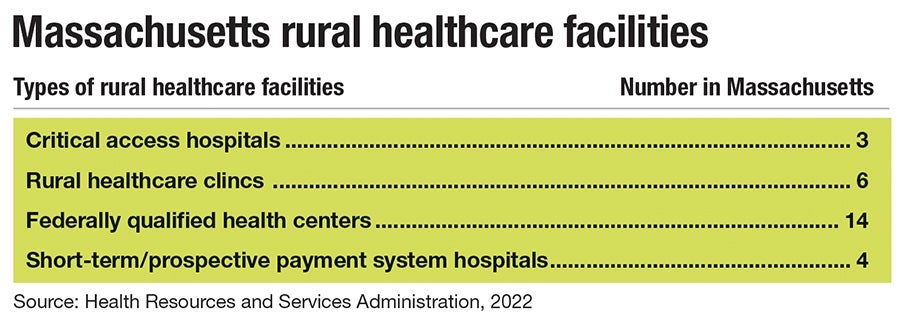
Massachusetts has a landmass of 7,800 square miles with most of its 7,029,917 population situated in cities and urban areas along the East Coast. Meanwhile, 105,884 people live in rural areas throughout Central and Western Massachusetts, according to the U.S. Department of Agriculture.

Technologies such as telehealth quickly adopted in the crisis situation of lockdowns have become healthcare models that are here to stay.
“Telehealth is a really nice perk that I think before the pandemic, we were not utilizing, literally very much at all, and now we are. So, that might be the silver lining in all of this is that we figured out how to meet patients kind of where they are in terms of being able to do some telemedicine with them if they can't come into the office in a physical way,” said Dr. Elizabeth Siraco, medical director of Milford Regional Physician Group.
Obstacles in rural healthcare
Dr. Kate McIntosh is the vice president and chief medical officer of Springfield-based insurer Health New England, which provides services in Worcester. Prior to joining Health New England in October, McIntosh had an 18-year medical career in Vermont and served as the only pediatrician in Benzie County, a rural area of Michigan from 1998 to 2004.

“Travel becomes an issue to get to healthcare services. In rural health care, there are fewer providers, and sometimes there are fewer hospitals; or the hospital that they have they have to go farther for to receive services like specialty care,” McIntosh said.
In addition to the transportation hurdles found in small towns disconnected from public transportation services, McIntosh said rural areas are susceptible to becoming food deserts, with a lack of access to healthy and affordable food options or grocery stores negatively impacting the population’s overall diet and health. This can be further exacerbated by lack of exercise opportunities and infrastructure such as sidewalks.
While the advent of telehealth has opened a whole new world of possibilities in medicine, rural communities are often unable to take advantage of this new technology due to broadband issues. Poor internet access or providers charging unaffordable prices for broadband can make even telehealth access challenging for those in remote areas of the state. For rural residents who lack internet access, telehealth can be administered via telephone.
“So it's not just technology, it's everything that impacts you when you live rurally,” McInstosh said. “In really rural communities, the other thing that is happening is there's more and more of a move toward human contact of sending people out to go find the folks who can't come in.”
New England Health’s Dispatch Health ambulance service goes out for non-urgent cases to meet people in their homes and administer medical services in both urban and rural areas.
Advancements like these in home health services are changing the game, said Siraco. Rather than having patients go to a hospital, nurses can be sent to a patient’s home where tests such as blood pressure can be administered while the results are reviewed by a doctor at another location. This new model of patient service is crucial, especially for individuals who find it difficult to leave their homes or lack transportation.
Another development is the ability for rural community hospitals to partner with larger hospitals for services such as e-ICU. For example, the smaller hospital could pay a larger hospital to help cover their ICU night shift and when a patient arrives the local nurses administer tests and aid while a doctor at a larger hospital provides expertise and diagnosis virtually through a screen. The e-ICU allows patients’ records and tests to be stored and then accessed remotely by doctors in other areas.
“It's pretty advanced and thrilling technology. It's been around for a while, but I think it's been more utilized since the pandemic,” Siraco said.

New technologies on the horizon
Starting as a paramedic in New Hampshire and the North Shore of Boston, Tim McGough in 2007 began working for ZOLL Medical Corp. in Chelmsford as an inventor for a patent called Pocket CPR. This pocket-sized CPR feedback device prompts the user through all the steps of CPR and helps determine effective chest compression depth.
After years of devoting his career to the development of the Pocket CPR, McGough’s 86-year-old father passed away from cardiac arrest on Nov. 6, 2020.
“He died on the steps of his front door 30 feet from one of these. And in the arms of my oldest brother, and my own brother didn't realize that there was a Pocket CPR 30 feet away from him. And that might have helped my older brother do better CPR or do CPR on my dad,” McGough said.
Dr. Beno Oppenheimer founded Relay Response, offering a smartwatch and downloadable software to provide real-time data to instruct wearers how to conduct CPR to maximize the likelihood of survival. The medical device is part of a partnership at UMass Memorial Health in Worcester in the Professional Apprenticeship Career Experience program. Dr. Chad Darling, who specializes in emergency medicine at UMass Memorial, is using Relay Response to teach high-risk cardiac arrest patients and their families how to administer CPR in case of a medical emergency.
Relay Reponse’s approval from the U.S. Food and Drug Administration is pending, so it is only allowed to be used as a training device among medical professionals; but once the device is cleared, the goal is to use the wearable watch to assist the general public in actual cardiac arrest rescues.
Meanwhile, another Worcester physician, Dr. Joe Sabato, who serves as 911 medical director at UMass Memorial Medical Center’s emergency department, is partnering with defibrillator and drone manufacturers to create a defibrillator delivery system to be dispatched to patients in emergencies and used to sustain a patient until EMS services arrive on scene.
Sabato had been working on the program during his time as a physician in Florida and is hoping to bring the EMS model to Massachusetts in an effort to greatly reduce the amount of time a person in cardiac arrest needs to wait to receive CPR assistance. The drones would be operated by CPR-instructed pilots who would be able to provide step-by-step CPR instructions to those on scene until paramedics arrive. The technology has already been used successfully in rural parts of Nevada and would be a great asset for EMS services in both rural and suburban parts of Massachusetts, said Sabato.
“The next wave of defibrillators will be drone-delivered defibrillators,” Sabato said.