The new program at UMass Memorial Health offers hospital-level care to patients in their own homes, using virtual monitoring systems and at-home visits from healthcare professionals.
Get Instant Access to This Article
Subscribe to Worcester Business Journal and get immediate access to all of our subscriber-only content and much more.
- Critical Central Massachusetts business news updated daily.
- Immediate access to all subscriber-only content on our website.
- Bi-weekly print or digital editions of our award-winning publication.
- Special bonus issues like the WBJ Book of Lists.
- Exclusive ticket prize draws for our in-person events.
Click here to purchase a paywall bypass link for this article.
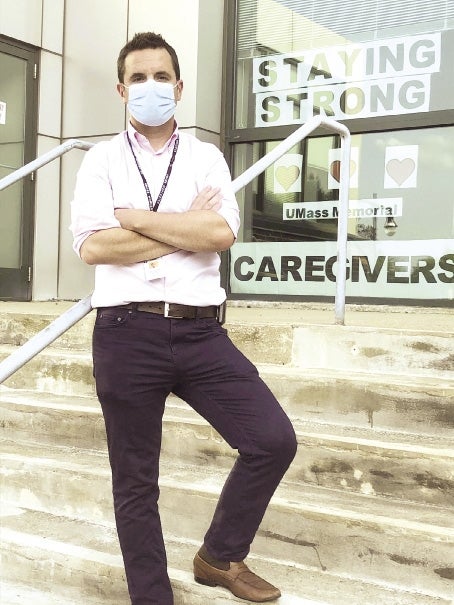
Dr. Constantinos “Taki” Michealidis started in July as the medical director of UMass Memorial Health’s new Hospital at Home program, which launched on Aug. 3. Dr. Michealidis has worked in the virtual healthcare field for four years at Atrius Health in Newton and Medically Home Group, Inc. in Boston. The new program at UMass offers hospital-level care to patients in their own homes, using virtual monitoring systems and at-home visits from healthcare professionals.
How has the field of virtual health care changed since you first started working in this industry?
At-home hospital care, in general, has been mostly used in international contexts for the last 70 years, and over about the last 30 years, a lot of the initial pioneering research on home hospital care came out. Over the last two years with the coronavirus pandemic, we’ve seen an explosion in virtual care. As folks have self-isolated and quarantined in their homes, we’ve really had a change in where people expect to get their care.
What are the benefits for patients getting care at home, rather than inside a hospital?
There’s some very concrete data suggesting if a patient is placed in a home hospital, there is about a 20% to 30% reduction in mortality and in readmissions, with very reassuring safety data. You don’t see falls or delirium or hospital-acquired infections in the home environment. You see a much lower probability the patient will be admitted to a skilled nursing facility after their home hospital stay, which is something all of us can sort of align on. Who would want for our mom or dad to avoid going to a nursing home?
How does UMass Memorial’s Hospital at Home program compare with other virtual healthcare programs you’ve worked on?
Having been involved in a number of other home hospital programs, UMass launched its program very quickly with a very strong focus on patient safety, and we’ve been admitting a little more frequently than a lot of the other programs do early on. Digitally, it’s a very progressive healthcare system. We’re doing things on day one of the program many other health systems struggle with. We have, for instance, continuous vital sign monitoring, while most programs start off with intermittent monitoring. That’s going to allow us to take a slightly sicker patient population.
How does the program address COVID-19?
We’re caring for patients with severe COVID in our home hospital program as we speak. Our goal is to be able to expand access for folks when our emergency department is super, super busy because of the increase in cases.
The coronavirus pandemic has highlighted the need for healthcare equity and accessibility. What is the process of getting admitted into this program, and how has UMass addressed accessibility?
There’s a real focus on accessibility, providing for the entire region of care, and caring for vulnerable populations in our home hospital program. Eric Dickson, the UMass Memorial Health president and CEO, is incredibly passionate about how large a vision this could be for our most vulnerable patient population. We’re only admitting patients where we think we can be as good as, if not substantially better than, the brick-and-mortar hospitals. We only admit patients who need hospital care, not urgent care or emergency department care. We have to make sure they live in our service area, which includes Worcester and Shrewsbury for the short term, though we hope to expand. And then we have to make sure they have a home, running water, and electricity.
This interview was conducted and edited for length and clarity by WBJ Staff Writer Katherine Hamilton.