
Worcester nonprofits work to educate their skeptical populations on the COVID vaccine
 PHOTO/Matt Wright
First responders receive the COVID vaccine at the Worcester Senior Center in January.
PHOTO/Matt Wright
First responders receive the COVID vaccine at the Worcester Senior Center in January.
When it comes to connecting vulnerable populations with healthcare services otherwise difficult or impossible to obtain, the Edward M. Kennedy Community Health Center in Worcester is well-versed.
For 49 years, those running the center and its satellite offices have made it their mission, serving nearly 29,000 patients, 90% of which are low-income, 71% of which belong to minority groups and 30% of which don’t have health insurance. Unprecedented times aside, the coronavirus vaccine rollout has been no exception.
But one very real challenge unique to vaccine distribution, both in Massachusetts and the rest of the country, has centered around overcoming skepticism and assuaging concerns about the relative safety of inoculation.

“Like statistics would tell you – and we talked a lot about this health as a healthcare profession over the last few months – communities of color have had a historic hesitancy to vaccinations like this due to, frankly, a really dark history of testing and experimenting,” said Stephen Kerrigan, president and CEO of the Edward M. Kennedy Community Health Center.
The center has been working to reduce that hesitancy, and Kerrigan said he thinks that work is paying off.
“As soon as we knew vaccines were coming, [there has been an] effort to educate our patients on what it means, the value of getting it,” Kerrigan said. “And it continues, by the way, to this day.”
Demystifying and educating the patient population about the vaccine’s safety and efficacy is a multilateral project both in the center and the community, Kerrigan said, noting the organization has processes in place both internally and externally, working with the City of Worcester, nonprofit partners, elected and appointed officials to drum up educational initiatives.
One of the key internal decisions aimed at assuaging concerns about the vaccine included mandating most staff at the health center received the vaccine, a process which began in December. To date, the policy has resulted in 97% of the roughly 375 employees at Kennedy already vaccinated against the COVID-19.
“We wanted to make sure, as we provide health care for more vulnerable and at risk populations, we wanted to make sure that we sort of lead with our own value sets and could show by example, why the vaccine is really important,” Kerrigan said.
Other steps the center is taking include calling vaccine eligible population groups to discuss their options and answer questions – in a language they’re comfortable communicating with. Some 92 languages are spoken by the health center’s patients, Kerrigan said, so recruiting bilingual and multilingual staff has also been part of the outreach.
Waiting game
At Spectrum Health Systems, which serves patients with substance abuse and mental health disorders, the vaccine rollout has been largely successful, pulling on data from its first six weeks, beginning at the end of January.

“We haven’t seen a positive case in about a month,” said Kristin Nolan, senior vice president of behavioral health at the Worcester organization.
That varies significantly from the end of last year, when, said Nolan, infection rates in their facilities surged in alignment with state trends.
Spectrum has been working directly with the state rollout since early January, Nolan said, when the system, which employs healthcare workers trained to give shots, began vaccinating direct care staff. While Spectrum didn’t mandate the vaccine for its employees, she estimated between 60 and 70% of staff have been inoculated on-site, with additional others vaccinated at outside clinics.
“We were pleased with the amount of staff who wanted to receive this vaccine because ultimately provides a safer environment to our patients,” Nolan said. “The more people that we vaccinate, the safer work environment is going to be.”
Patients began receiving vaccines by the beginning of February, when the Massachusetts Department of Public Health made them accessible to people living in congregate care settings. Similarly to the Kennedy Community Health Center, Nolan said some of their patients were hesitant, especially at first.
“This wasn’t mandatory for those populations,” Nolan said. “I would say at first … folks were weary, asking a lot of questions. [They] wanted to wait and see.”
Through education, and over time, however, hesitant patients started to come around.
“More recently, we’ve had a lot of interest in getting a vaccination,” Nolan said. “When we have it available, we’re filling up sign-up sheets. I think it’s like everything else, with the unknown and so then just the education, giving patients the opportunity to meet with our own nursing staff, and then the physician at the time, at the clinic really reassured people.”
New science, but more effective
When it comes to fighting misconceptions about the safety and efficacy of the coronavirus vaccines, fears abound, both inside and outside of vulnerable population groups. Dr. Robert Finberg, distinguished professor of medicine, infectious disease expert and chair emeritus at UMass Medical School in Worcester, has heard an array of incorrect rumors about the vaccines available, including they cause infertility, or they have a negative effect on those who have already had COVID-19.

Neither of these rumors have supporting evidence, he said.
Nor is it true the research behind the first two coronavirus vaccines to receive approval from the U.S. Food and Drug Administration – mRNA vaccines from Pfizer and Moderna – is as new as some people think.
“The research has been done over the last decade or so,” Finberg said. “It’s just beginning to come out.”
That said, in the grand scheme of history, the Pfizer and Moderna coronavirus vaccine model is new-ish, utilizing mRNA to trigger an immune response rather than a dead or weakened virus injections, like many other vaccines people may have encountered over the years. Research around mRNA vaccines has taken place for years, said Finberg, but the push to bring that research to fruition picked up speed when it became clear that the coronavirus pandemic was unravelling into an emergency.
“People say this is a new vaccine. Well, not really, it just wasn’t licensed until now,” Finberg said. “It’s fairly new technology, but it’s years old.”
Plus, Finberg said, the Pfizer and Moderna options are actually significantly more effective than virtually any other common vaccine.
“These vaccines are over 95% effective in preventing disease,” Finberg said. “They were tried in large trials and previous vaccines have sort of been done hit or miss, and we don’t know what they’re effectiveness is in general. These are just much better vaccines.”
A third vaccine to receive approval from the FDA, made by Johnson & Johnson, is a viral vector vaccine, which, according to the U.S. Centers for Disease Control, utilizes a modified virus to deliver genes which then instruct cells to make antigens. That vaccine has been reported to be up to 72% effective.
All three FDA-approved vaccines, including Johnson & Johnson, were found effective in significantly reducing hospitalizations from COVID-19.
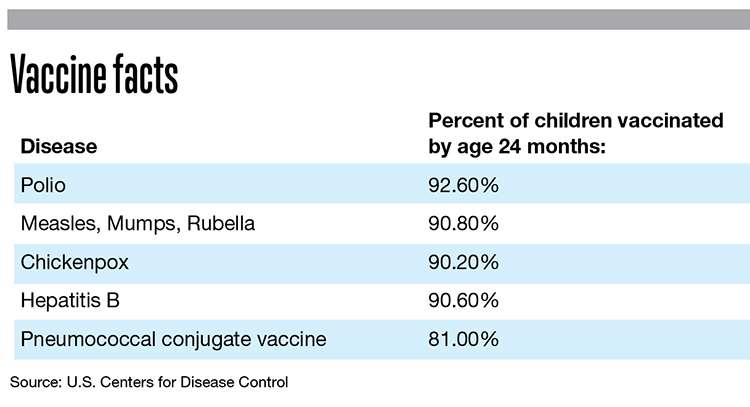
For comparison, the CDC reports the seasonal flu virus reduces the risk of illness between 40% and 60% among the overall population during years when the vaccine matches the circulating flu variation.
The challenge, then, for healthcare providers and community leadership lies in messaging and outreach. The data is there, public perception just needs to catch up with it.
“It isn’t like this vaccine was rushed to market. It wasn’t,” Finberg said.
WBJ Web Partners
No one in America should ever be "mandated" to have foreign material injected into their bodies! Last I knew we had freedom of choice in the United Stated. People should be able to make their own decisions about the COVID vaccine without being pressured or shunned or guilted.












1 Comments