In a flash this spring, Reliant Medical Group in Worcester was suddenly using video and phone technology to have patients meet with health providers for about a quarter of the visits that used to take place in person.
Get Instant Access to This Article
Subscribe to Worcester Business Journal and get immediate access to all of our subscriber-only content and much more.
- Critical Central Massachusetts business news updated daily.
- Immediate access to all subscriber-only content on our website.
- Bi-weekly print or digital editions of our award-winning publication.
- Special bonus issues like the WBJ Book of Lists.
- Exclusive ticket prize draws for our in-person events.
Click here to purchase a paywall bypass link for this article.
In a flash this spring, Reliant Medical Group was suddenly using video and phone technology to have patients meet with health providers for about a quarter of the visits that used to take place in person.
It wasn’t just Worcester-based Reliant wasn’t using telehealth much before. It wasn’t at all. The company had only done a pilot program with older patients to see how well technology could be used with patients who might have a harder time making it to a doctor’s office.
With the coronavirus pandemic, of course, Reliant and healthcare providers everywhere were forced to quickly change course.
“We literally turned this on in two days,” said Dr. Larry Garber, Reliant’s medical director for informatics.
Just like that, 500 providers have used telehealth to meet electronically with patients, he said.
“It was thrust upon them very quickly, and they adapted to it,” Garber said.
The same could be said for practitioners and patients virtually everywhere during a time when it suddenly wasn’t advisable to go to a doctor’s office unless absolutely needed. In UMass Memorial Medical Center’s outpatient services, 23,000 to 25,000 telehealth appointments were conducted in May alone. That’s up from just about 40 over a whole year before – a rate of about one for every 30,000 appointments.
Now, healthcare leaders in Central Massachusetts who oversee such details are looking ahead to see how much telehealth is here to stay.
“I’d love to know the answer to that question, as would everybody,” said Dr. Patrick McSweeney, the president of the Milford Regional Physician Group.
Dr. David Smith, the associate vice president of virtual medicine at UMass Memorial, was more confident. A UMass Memorial patient survey found 42% to have done a virtual visit, he said. Two-thirds would do it again.
“Telehealth is here to stay,” Smith said. “COVID was the shot in the arm it needed.”
Technological and trust hurdles
The technology has long been in place to have doctors and patients meet electronically when making it to an office would be difficult or a certain specialist was far away.
Doctors and other providers have been used to meeting with patients one day – face-to-face – their whole careers, which in some cases span decades. Older patients were also less anxious to figure out technology needed to meet with a provider in a whole new way.
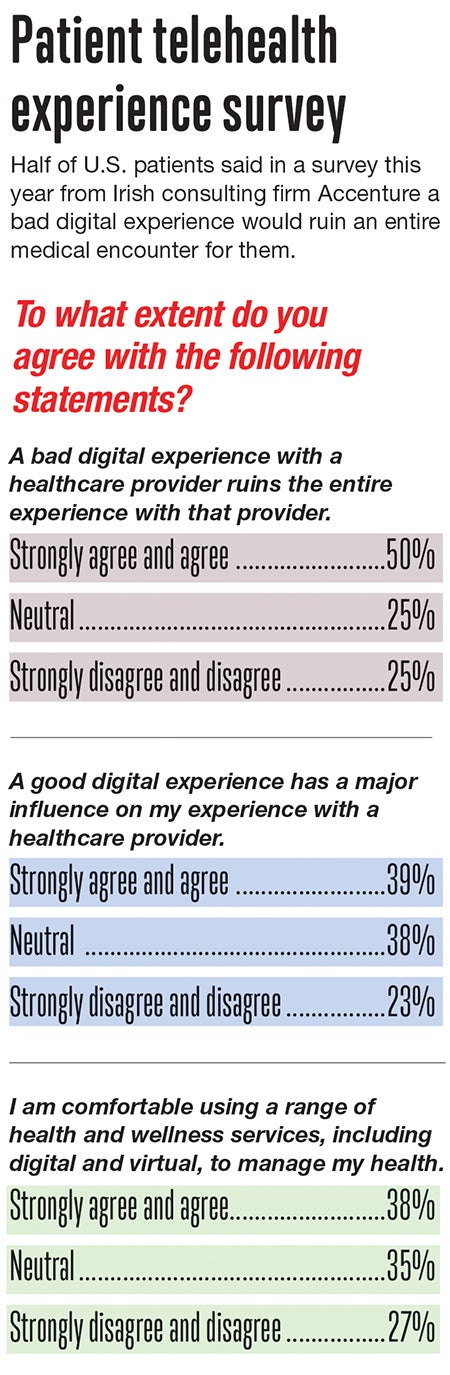
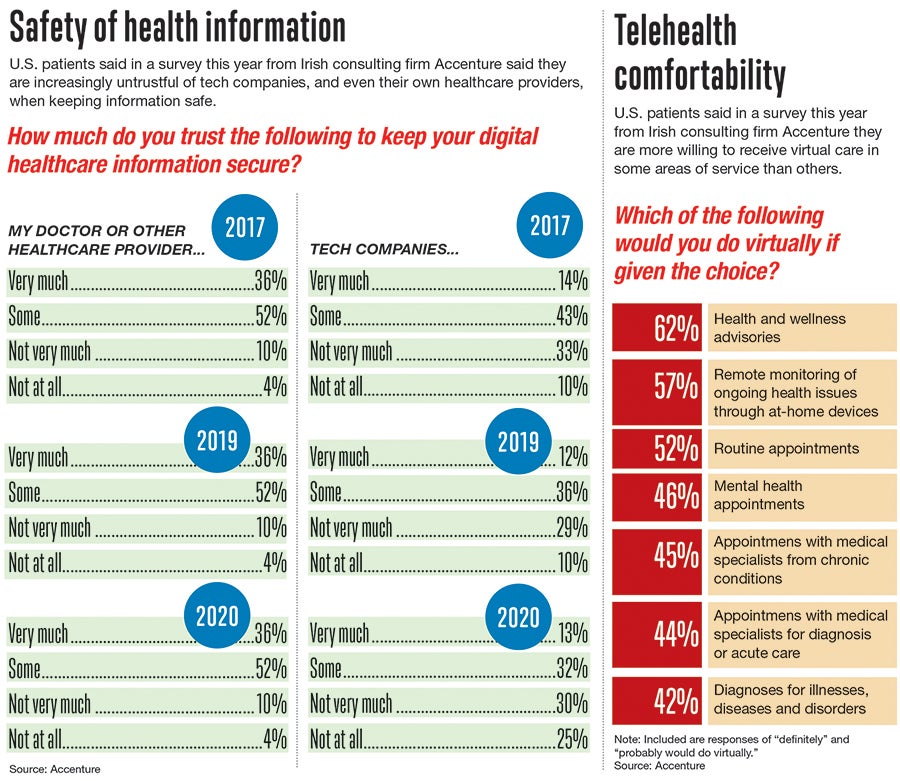
Patients have been shown to be quickly deterred by bad telehealth visits and have a lack of trust in the safety of their information online.
Half of patients in a survey this year by Accenture, a professional services company, said a bad digital experience with a healthcare provider would ruin the whole experience with that provider.
But there is a more encouraging trend for those looking to adapt telehealth practices.
While 14% of the Silent Generation and 20% of Baby Boomers said they trust tech companies’ health services, those rates were 32% for Generation X and 43% for Millennials, younger generations who have been using technology for a greater share of their lives. Younger generations showed more willingness to try virtual care from tech companies and retail brands.
After the peak of the pandemic, healthcare providers haven’t seen a lack of trust – at least for now – standing in the way of telehealth becoming a greater part of health services permanently.
At Saint Vincent Hospital in Worcester, health leaders cite other challenges patients and practitioners have had to overcome.
“A lot of it is a perception that ‘A doctor needs to see me,’” said Dr. Sowmya Viswanathan, the chief medical officer for Saint Vincent and sibling hospital MetroWest Medical Center. “Meaning, he or she needs to see me in person in order to diagnose me properly.”
Among practitioners, some had concerns about missing physical cues like an unsteady gait or that the appointment would feel less personal, said Dr. Melissa Buchner-Mehling, the medical director for advisory services for Saint Vincent. But providers have also discovered telehealth can increase efficiency, she said. Patients who before might have difficulty scheduling an appointment around work or child care can now more easily be seen.
Making telehealth work
Dr. Joseph Kvedar, the president-elect of the American Telemedicine Association, said he’s advised clinicians to stay mindful of what lends itself to online appointments and what doesn’t.
“If we stray into areas where a physical exam is needed – where I have to touch you or use an instrument to get the information I need to make the diagnosis – and we don’t do that, then quality will suffer,” he said in a forum by the Betsy Lehman Center for Patient Safety, a state office in Boston.
Another factor could dictate the longer-term widespread use of telehealth: health insurance reimbursement rates.
Today, insurers and Medicaid and Medicare are paying the same rates for telehealth as for in-person appointments. That wasn’t the case before. Healthcare systems faced a financial disincentive for switching to telehealth.
“That was one of the larger reasons why adoption lagged where the technology was,” said Dr. Mark Manning, the medical director for ambulatory services at UMass Memorial.
Telehealth isn’t replacing services requiring in-person visits, like a CT scan, or MRI. But technology is already making some services available remotely, including a gadget acting like a stethoscope to analyze breathing.
Telehealth has worked best in areas such as behavioral health, which doesn’t require a physical touch, and dermatology, when a photo from a patient can often work just as well.

“There’s always going to be some limitation with technology,” said Dr. Basava Vallabhaneni, the system medical director for sound physicians and medical director of informatics at MetroWest Medical Center in Framingham and Natick. “Technology isn’t going to replace the physician-patient relationship. It’s going to complement it.”
At Reliant, Garber said telehealth is bound to be used at least slightly less once the pandemic passes. Garber, a practicing internist, predicted 10% to 20% of appointments will remain online. An annual physical, for example, could take place partly online with a briefer in-person visit for any needed hands-on exams.
UMass Memorial found itself fortunate to have built a telehealth platform integrated into Epic, the electronic patient record system it launched in 2017. When it quickly switched to telehealth during the pandemic, everything ran relatively smoothly.
“We were in a very good position when this hit to not have to work out those details in the midst of a crisis,” Smith said.

